Researchers from Auburn University, partnering with the University of Basel in Switzerland, have discovered a new way to make a cancer-targeting protein complex more stable, opening doors to better cancer treatments. Led by Dr. Rafael Bernardi from Auburn’s Department of Physics and Dr. Michael Nash from the Department of Chemistry at the University of Basel, the study focuses on PD-L1, a protein that tumors use to hide from the immune system.
In many cancers, PD-L1 acts as a “shield,” binding to immune cells and signaling them to ignore the cancer, allowing the tumor to grow undetected. By blocking PD-L1, treatments can help the immune system recognize and attack cancer cells more effectively.
In this study, the researchers investigated the PD-L1 interactions with a small protein called an “Affibody,” which is designed to stick to cancer cells and help carry cancer-fighting drugs directly to the tumor. Together, these two proteins could make it easier to deliver treatments exactly where they’re needed, making cancer therapies more effective and reducing side effects on healthy cells.
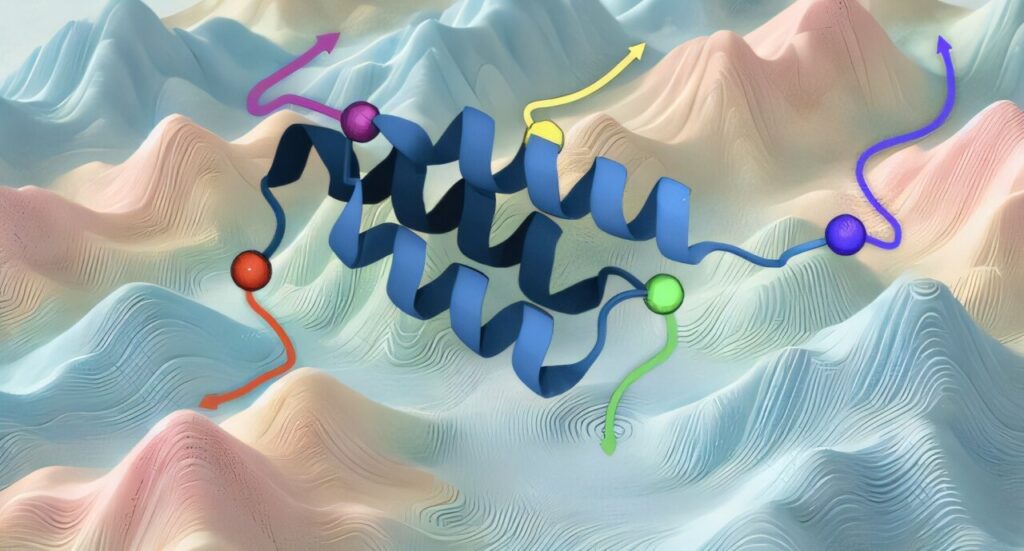
Published in ACS Nano, the study introduces the concept of “force anisotropy,” demonstrating how the strength of the PD-L1 and Affibody pairing varies based on specific attachment points. The team discovered that adjusting the attachment points on PD-L1 could make this pair up to four times stronger.
“This breakthrough could improve how we attach drugs to proteins like Affibodies so they can find and bind to cancer cells effectively,” said Dr. Diego Gomes, a postdoctoral researcher at Auburn.
Dr. Bernardi explained, “By adjusting where we attach Affibodies, we can make them stronger so they stay intact in the body longer, helping them reach cancer cells more effectively.”
The team used both lab experiments and computer models to test how well the protein complex could hold together. They found that with the right adjustments, the complex not only held strong but even grew more stable under tension, making it ideal for carrying treatments directly to cancer cells.
This discovery could lead to more reliable drug delivery systems, allowing researchers to develop cancer therapies that target tumors more precisely and stay effective longer. Dr. Bernardi’s team is now looking to design even stronger Affibody proteins that can find and attach to different cancer types with greater accuracy.
Beyond drug delivery, this work may also help in cancer surgery, where Affibodies can carry dyes to make cancer cells glow under special lights, helping surgeons spot and remove tumors. They could also be loaded with radiation to directly target and kill cancer cells over time.