The spongelike structure of metal-organic frameworks (MOFs) allows these polymers to possibly carry and deliver a range of therapeutic compounds. Now, researchers reporting in ACS Applied Bio Materials have treated a chromium-containing MOF with a dose of acetic acid, more concentrated than in vinegar, to expand its pore size and surface area. The puffed-up MOF held more ibuprofen or chemotherapy drug than the original version and showed improved performance as a potential drug-delivery vehicle.
Taking medications by mouth is a convenient way to administer pharmaceuticals. However, this method sometimes involves ingesting several pills per day, or requires large pills that can be difficult to swallow. So, researchers are investigating how to use MOFs for drug delivery to minimize dosing frequency and maximize treatment efficiency. By customizing the polymers’ pore sizes and structures, scientists have created nanoscale vehicles that may offer more controlled and targeted drug release.
However, to carry and deliver even more drug molecules, the pores would need to expand further than current versions can. A research team led by Fateme Rezaei at the University of Miami wanted to optimize an existing MOF and improve the polymer’s delivery of two common therapeutics of different molecular sizes: the anti-inflammatory drug ibuprofen and a smaller compound 5-fluorouracil, a chemotherapy drug used to treat cancer.
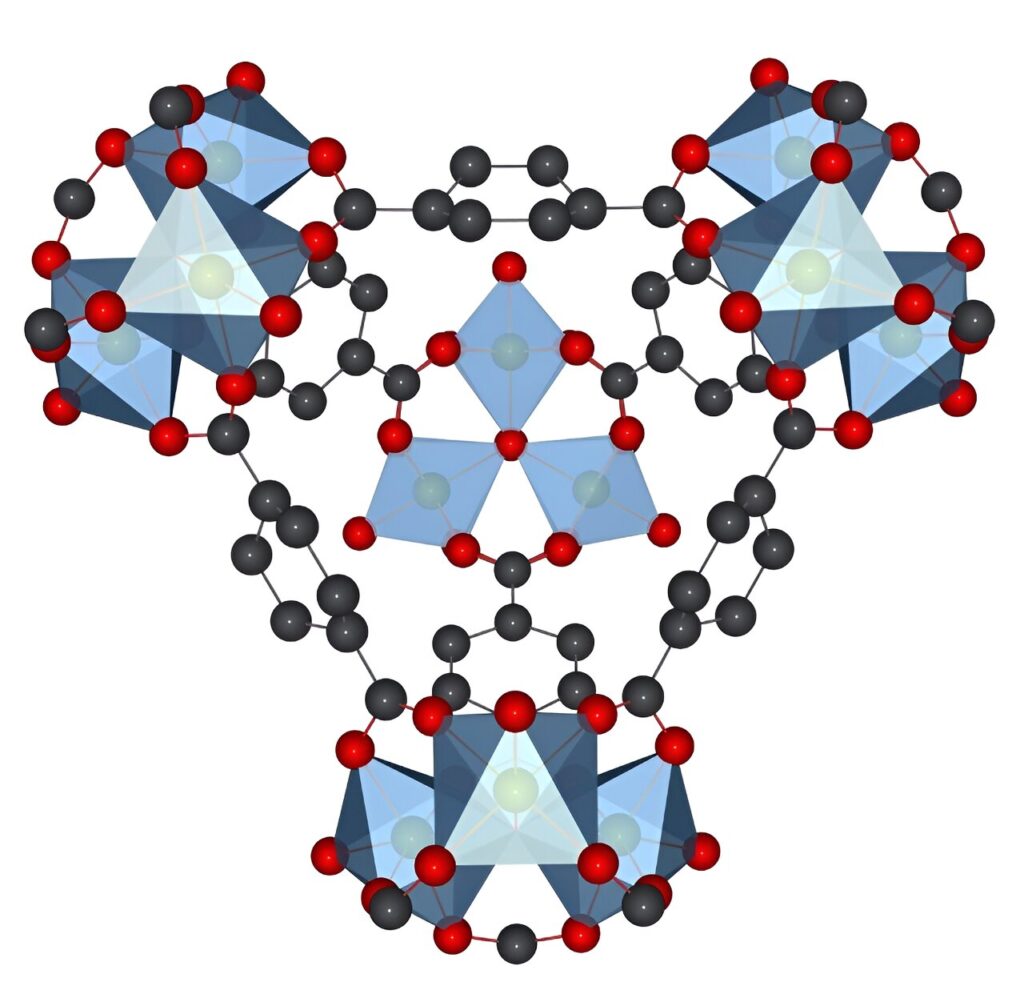
They started with an established method to synthesize a biocompatible chromium-containing MOF and added a step with an acetic acid rinse. The acid caused the polymer’s pores to expand from about 2.5 nanometers (nm) to 5 nm wide. In laboratory experiments to characterize the MOF’s drug-loading capability, the researchers observed that the puffed-up version took in more ibuprofen and 5-fluorouracil molecules than the chromium-containing framework with standard-sized pores.
Then, in drug-delivery experiments, they loaded the pore-expanded and standard MOFs with either ibuprofen or 5-flurouracil and measured how quickly the drugs passed into a saline solution. Rezaei and colleagues found that the new frameworks released both drugs substantially faster than the original ones. The researchers attributed the higher drug loading and release rates to the larger pores and surface area of the expanded framework, which provides larger “doors” for the drug molecules to enter and exit through.
Simple changes such as these could maximize the effectiveness of MOFs in future drug-delivery applications, the researchers say. As a next step, they plan to determine how slow and progressive drug release within specified time frames can be achieved by modifying MOF pore structure.