Researchers at the Icahn School of Medicine at Mount Sinai have designed a regenerative medicine therapy to speed up diabetic wound repair. Using tiny fat particles loaded with genetic instructions to calm down inflammation, the treatment was shown to target problem-causing cells and reduce swelling and harmful molecules in mouse models of damaged skin.
Details on their findings were published in a paper titled “Accelerating diabetic wound healing by ROS-scavenging lipid nanoparticle-mRNA formulation” in the May 20 online issue of the Proceedings of the National Academy of Sciences.
Diabetic wounds, often resistant to conventional treatments, pose serious health risks to millions of people worldwide. Immune cells known as macrophages, which are supposed to help, end up causing inflammation instead. This inflammation harms other cells and makes it harder for the wound to heal properly and quickly.
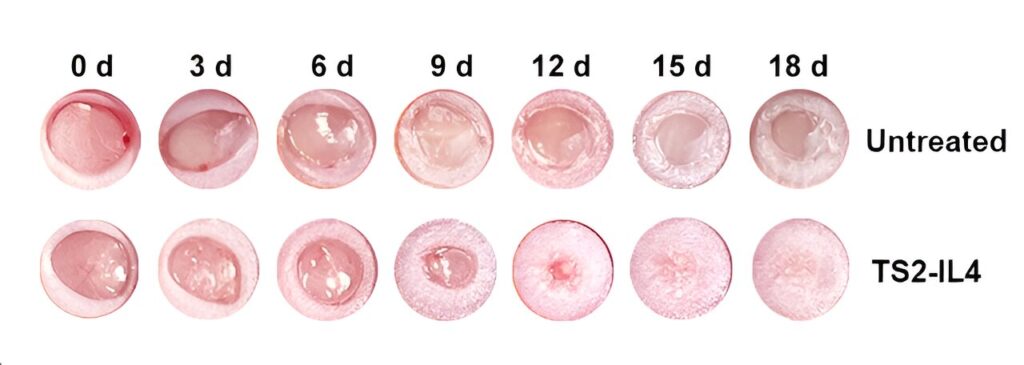
Using lipid nanoparticles (LNPs) loaded with RNA encoding IL-4, a cell-to-cell signaling protein known as a cytokine, the therapy targeted dysfunctional macrophages while simultaneously reducing inflammation and “reactive oxygen species” (ROS) in diabetic wounds.
ROS molecules are produced naturally in the body during various metabolic processes and play roles in cell signaling and immune responses. However, excessive ROS production can lead to oxidative stress, causing damage to cells, proteins, and DNA. This stress is associated with various diseases and conditions, including inflammation and aging.
“In preclinical models, we basically showed the therapy’s ability to reprogram pro-inflammatory macrophages into reparative ones, leading to improved wound healing outcomes,” says Yizhou Dong, Ph.D., corresponding author of the study, Professor of Immunology and Immunotherapy, and a member of the Icahn Genomics Institute and the Marc and Jennifer Lipschultz Precision Immunology Institute at Icahn Mount Sinai.
“Dysfunctional macrophages drive diabetic non-healing wounds, but we can reprogram them to stop the damage and instead help the healing process. We aim to promote faster and more effective wound closure by reprogramming these cells and modulating the inflammatory environment.”
Earlier this year, in a related study, Dr. Dong and colleagues reported on lipid nanoparticles that enhanced the tissue engineering and regeneration activity of adipose stem cells for treating diabetic wounds (Nature Communications).
While the results of the current study are encouraging, the researchers emphasize the need for a rigorous randomized controlled clinical trial to confirm safety and efficacy in humans.
“Our ultimate goal is to translate these findings into tangible benefits for diabetic patients. With further research and validation, this RNA-LNP therapy could potentially revolutionize diabetic wound management with one easily scalable application of a comparatively inexpensive therapeutic agent,” says Dr. Dong.
“The study also suggests the potential for RNA-LNP therapeutics to be more generally designed to reprogram disease-causing macrophages in an organism, as pro-inflammatory macrophages are implicated in a wide range of diseases.”