Diabetes, a widespread condition affecting approximately 13% of American adults, is often accompanied by complications such as impaired wound healing. If left unchecked, this can lead to severe outcomes, including the need for amputation.
The challenge of finding effective treatments for diabetic wounds has grown increasingly urgent. Such wounds are marked by prolonged inflammation, lack of oxygen, and disrupted blood vessel formation, which all contribute to delayed recovery. However, a new frontier in biomedical research is pointing toward exosomes as a potential solution.
A team from NYU Langone and NYU Tandon including Jin Kim Montclare has begun to explore exosomes, tiny membrane-bound vesicles, as promising tools for healing. These nanovesicles carry various biological materials—nucleic acids, proteins, and lipids—allowing them to mediate intercellular communication and influence processes such as tissue repair.
The findings are published in the journal ACS Applied Bio Materials.
Specifically, exosomes derived from mesenchymal stem cells (MSCs), including those from adipose tissue, have demonstrated significant potential in promoting wound healing in animal models. Their therapeutic effects appear to stem from their ability to reduce inflammation and promote a healing-friendly environment by enhancing blood vessel formation and encouraging the activity of cells like fibroblasts and endothelial cells, which are essential for tissue repair.
One major advantage of exosomes is their ability to bypass some of the risks associated with traditional stem cell therapies, such as uncontrolled cell growth or immune rejection. However, despite their promise, exosomes typically require repeated administration—either through subcutaneous or intravenous injections—which poses a challenge for long-term wound management.
Montclare’s team have been exploring innovative ways to enhance the therapeutic potential of exosomes, one of which involves combining them with hydrogels. Hydrogels, composed of networks of cross-linked polymers, can encapsulate exosomes within their structure. This encapsulation enables a more sustained and localized release of exosomes directly at the wound site, without the need for invasive injections.
Hydrogels are already recognized for their biocompatibility and ability to hydrate wounds, making them useful as wound dressings on their own. When combined with exosomes, their therapeutic effectiveness increases significantly, especially for diabetic wounds.
Recent studies have shown that hydrogel-exosome combinations consistently lead to faster wound closure than either hydrogels or exosomes used alone. These hydrogel systems are not protein-based, but recent advances in protein-based hydrogel technology have opened new possibilities for improving wound healing.
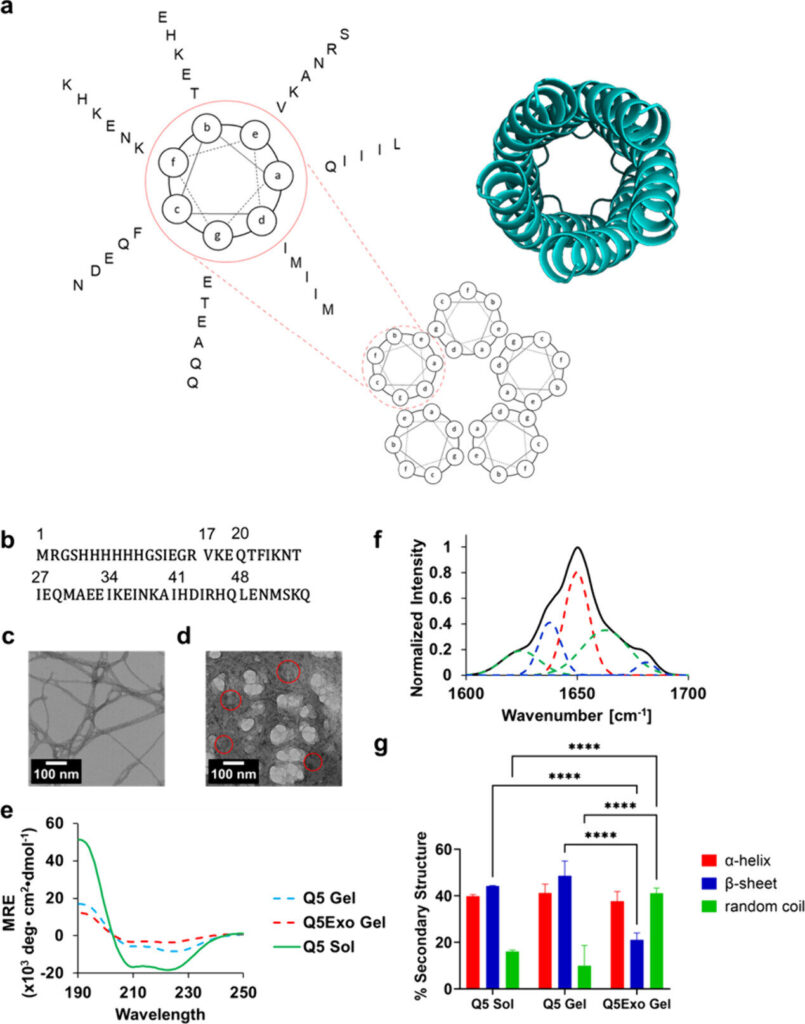
Montclare has developed a protein-based hydrogel, referred to as “Q,” which forms a gel at low temperatures through a process called upper critical solution temperature (UCST) gelation. This protein-based hydrogel self-assembles into nanofibers, forming a physically cross-linked network that provides mechanical strength.
By fine-tuning the protein sequence using advanced computational tools, such as the Rosetta score and Poisson-Boltzmann electrostatic potential calculations, they have been able to improve the gel’s mechanical properties, stability, and speed of formation—key factors in creating an ideal wound dressing.
To push this approach further, they designed a variant of the Q hydrogel, dubbed Q5, using automated selection methods to optimize its stability. They encapsulated exosomes within Q5 to create a new hydrogel-exosome system, called Q5Exo. This system offers a topical, noninvasive wound dressing that holds promise for treating diabetic wounds more effectively than traditional methods, which rely on injections.
In studies using diabetic mouse models, Q5Exo demonstrated a significant reduction in healing time when applied topically compared to exosomes administered via injection. This suggests that protein-based hydrogels, with their tunable properties, could become a powerful platform for enhancing wound healing outcomes in diabetes.
As research continues, such hydrogels could pave the way for a new generation of biocompatible, efficient wound dressings that harness the therapeutic power of exosomes.