A nanosized polymer, developed by a research team from Ben-Gurion University of the Negev, can selectively deliver chemotherapeutic drugs to blood vessels that feed tumors and metastases and has emerged as an effective treatment for advanced cancer. The polymer eliminates colorectal cancer liver metastases and prolongs mice survival after a single dose therapy.
Colorectal cancer (CRC) is the third most diagnosed cancer and the third most common cause of cancer-related death in both men and women in the United States. The liver is the most common site for CRC metastasis, with around 70% of patients ultimately developing liver metastases.
Treatment options for metastatic disease are scarce, and while surgery remains the gold standard, many patients need additional therapies (chemotherapy, targeted, or immune therapy) for a curative-intended treatment.
Targeted therapies and immunotherapies directed against specific features of the tumor have emerged as promising therapeutic strategies for cancer patients, but their efficacy is often limited by the large variety of mutation profiles of CRC tumors, many of them conferring resistance to specific treatments.
Conventional small molecule cytotoxic treatments show major drawbacks, such as lack of tumor specificity and toxicity to normal (healthy) tissues, short duration of effect, and treatment failure due to acquired drug resistance.
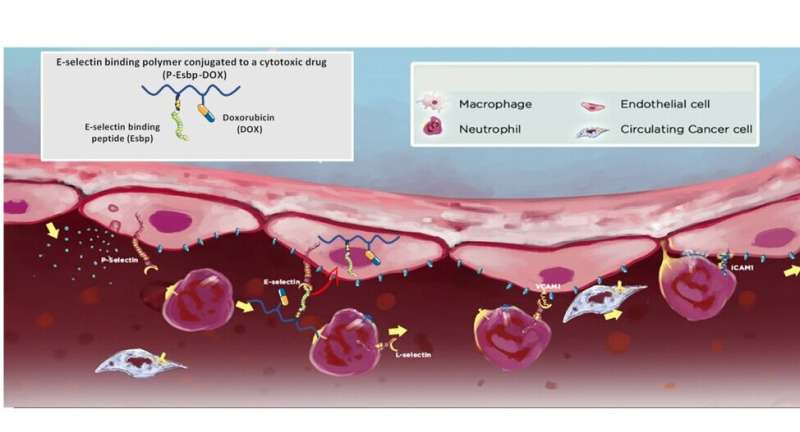
Prof. Ayelet David and her research team developed a tiny polymer (2–5 nanometers in size) for delivering chemotherapeutic drugs into endothelial cells at the inner lining of blood vessels that support tumor growth. The polymer carries a targeting peptide that binds to the adhesive molecule E-selectin, which is expressed exclusively on endothelial cells of new blood vessels that are created to feed growing tumors and thus can deliver drugs selectively to tumors and metastatic sites.
Once the polymer binds and enters the endothelial cells, it releases the toxic drug, thereby damaging the blood supply to growing tumors and metastases. Since the polymer is much larger in size than conventional chemotherapeutic molecules, it cannot leak from blood vessels to reach other healthy tissues, and thus significantly reduces the risk of side effects of chemotherapy drugs.
Previous studies conducted in Prof. David’s laboratory have shown that the unique polymer slows the progression of solid Lewis Lung Carcinoma tumors and significantly prolongs the survival time of mice with melanoma (skin cancer) metastases in the lungs.
In a recent study, Marie Rütter, a doctoral student from Prof. David’s research group, demonstrated that the polymer is not only effective in treating solid tumors but can cure mice with colorectal cancer metastases that have already spread to the liver. These findings were published in Nano Today.
About half of the mice that presented a significant number of CRC liver metastases fully recovered from the disease after a single dose of polymer therapy, and the long-term survival time of the mice was doubled compared to mice treated with a conventional chemotherapy drug.
“Colon cancer is a very aggressive tumor and spreads very quickly to the liver. About 25% of the patients with CRC present liver metastases at the time of diagnosis,” Prof. David explained.
“The available personalized treatments may prolong survival and improve quality of life for many patients with metastatic disease, although a cure is rare, and recurrence is expected. Our unique polymer demonstrates promising preclinical results for treating advanced cancer that has spread to other places in the body and usually cannot be cured or controlled with other therapies.”
“About 50% of mice with established colorectal cancer liver metastases survived after a single dose treatment, without presenting adverse effects. This is a remarkable advantage, indicating that the polymer accurately hits the target and eliminates the metastases from the liver of mice that responded well to the treatment.”
“These findings support the results of our previous studies, showing that a single dose treatment cures half of the mice with established melanoma lung metastases. The therapy does not require a pre-treatment assessment for gene mutations in tumors to achieve favorable clinical outcomes.”
So far, the research team has succeeded in validating treatment efficacy in various mouse models of cancer. The developed technology was recently licensed to a biomedical company (Vaxil Biotherapeutics) for further clinical development. The company is pursuing all the necessary steps to initiate human clinical trials as soon as possible.
“This is an excellent example of a fruitful collaboration between universities and the biotech industry to accelerate drug development,” said Dr. Galit Mazooz-Perlmuter, VP business development at BGN Technologies, the technology transfer company of Ben-Gurion University of the Negev (BGU). “This is exactly the way to turn scientific breakthroughs into technological advancements in Israel.”

