Drug delivery researchers at Oregon State University have developed a device with the potential to improve gene therapy for patients with inherited lung diseases such as cystic fibrosis.
In cell culture and mouse models, scientists in the OSU College of Pharmacy demonstrated a novel technique for the aerosolization of inhalable nanoparticles that can be used to carry messenger RNA, the technology underpinning COVID-19 vaccines, to patients’ lungs.
The findings are important because the current nebulization method for nanoparticles subjects them to shear stress, hindering their ability to encapsulate the genetic material and causing them to aggregate in certain areas of the lungs rather than spread out evenly, the researchers said.
The study led by Gaurav Sahay, a professor of pharmaceutical sciences, was published in ACS Nano.
Sahay’s lab studies lipid nanoparticles, or LNPs, as a gene delivery vehicle with a focus on cystic fibrosis, a progressive genetic disorder that results in persistent lung infection and affects 30,000 people in the U.S., with about 1,000 new cases identified every year.
One faulty gene—the cystic fibrosis transmembrane conductance regulator, or CFTR—causes the disease, which is characterized by lung dehydration and mucus buildup that blocks the airway.
Lipids are organic compounds containing fatty tails and are found in many natural oils and waxes, and nanoparticles are tiny pieces of material ranging in size from one- to 100-billionths of a meter. Messenger RNA delivers instructions to cells for making a particular protein.
With the coronavirus vaccines, the mRNA carried by the lipid nanoparticles instructs cells to make a harmless piece of the virus’ spike protein, which triggers an immune response from the body. As a therapy for cystic fibrosis, the genetic material would fix the flaw in patients’ CFTR gene.
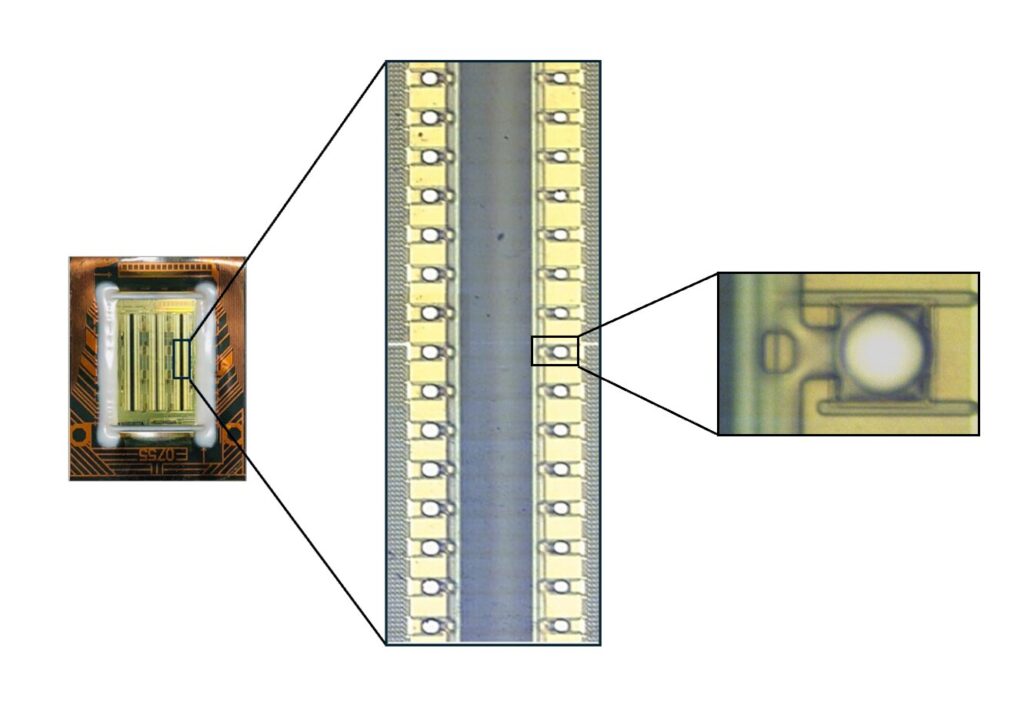
“We utilized a novel microfluidic chip that helps in generation of plumes that carry nanoparticles and does not cause any shear stress,” Sahay said. “This device is based on the similar idea of an ink-jet cartridge that generates plumes to print words on paper.”
Four years ago, Sahay said, an Oregon-based startup called Rare Air Health Inc. contacted him about the prospect of using microfluidic technology for the aerosolization and delivery of lipid nanoparticles.
Microfluidics is the study of how fluids behave as they travel through or are confined in microminiaturized devices equipped with channels and chambers. Surface forces as opposed to volumetric forces dominate fluids at the microscale, meaning fluids act much differently there than what is observed in everyday life.
“When Rare Air came to me, I thought the device might work great for our purposes, and what followed were extensive studies that demonstrated the superiority of this device in generating aerosolized nanoparticles as compared to clinically used vibrating mesh nebulizers,” Sahay said.
“The device does not let the nanoparticles aggregate and can deliver mRNA with higher precision than existing tech. The additional cool thing is that this device can be digitally controlled, and Rare Air is developing prototypes for human use.”
In addition to Sahay, the other Oregon State researchers on the study were Yulia Eygeris, Jeonghwan Kim, Antony Jozić and Elissa Bloom. Scientists from Funai Microfluidic Systems of Lexington, Kentucky, were also part of the collaboration.
“Funai focuses on inkjet tech and building these chips at scale; they worked closely to enable the device to be suitable for aerosolization,” said Sahay, who in addition to his role at OSU serves as an advisor and consultant to Rare Air. “This study demonstrates a marriage between new devices and formulation science that might hugely impact human health.”