Human mini-lungs grown by University of Manchester scientists can mimic the response of animals when exposed to certain nanomaterials. The study is published in Nano Today.
Though not expected to replace animal models completely, human organoids could soon lead to significant reductions in research animal numbers, the team led by cell biologist and nanotoxicologist Dr. Sandra Vranic argues.
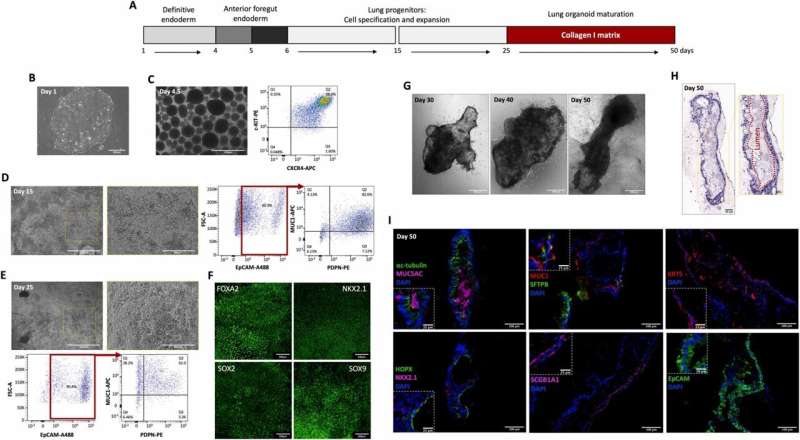
Grown in a dish from human stem cells, lung organoids are multicellular, three-dimensional structures that aim to recreate key features of human tissues such as cellular complexity and architecture. They are increasingly used to better understand various pulmonary diseases, from cystic fibrosis to lung cancer, and infectious diseases including SARS-CoV-2.
However, their ability to capture tissue responses to nanomaterial exposure has until now not been shown. To expose the organoid model to carbon-based nanomaterials, Dr. Rahaf Issa, lead scientist in Dr. Vranic’s group, developed a method to accurately dose and microinject nanomaterials into the organoid’s lumen. It simulated the real-life exposure of the apical pulmonary epithelium, the outermost layer of cells lining respiratory passages within the lungs.
Existing animal research data has shown that a type of long and rigid multi-walled carbon nanotubes (MWCNT) can cause adverse effects in lungs, leading to persistent inflammation and fibrosis—a serious type of irreversible scarring in the lung.
Using the same biological endpoints, the team’s human lung organoids showed a similar biological response, which validates them as tools for predicting nanomaterial driven responses in lung tissue. The human organoids enabled better understanding of interactions of nanomaterials with the model tissue, but at the cellular level.
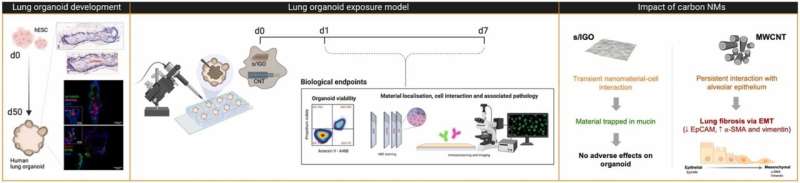
Graphene oxide (GO), a flat, thin and flexible form of carbon nanomaterial, was found to be momentarily trapped out of harm’s way in a substance produced by the respiratory system called secretory mucin. In contrast, MWCNT induced a more persistent interaction with the alveolar cells, with more limited mucin secretion and leading to the growth of fibrous tissue.
In a further development, Dr. Issa and Vranic based at the University’s Center for Nanotechnology in Medicine are now developing and studying a ground-breaking human lung organoid that also contains an integrated immune cell component.
Dr. Vranic said, “With further validation, prolonged exposure, and the incorporation of an immune component, human lung organoids could greatly reduce the need for animals used in nanotoxicology research.
“Developed to encourage humane animal research, the 3Rs of replacement, reduction and refinement are now embedded in UK law and in many other countries.
“Public attitudes consistently show that support for animal research is conditional on the 3Rs being put into practice.”
Professor Kostas Kostarelos, Chair of Nanomedicine at the University said, “Current ‘2D testing’ of nanomaterials using two-dimensional cell culture models provide some understanding of cellular effects, but they are so simplistic as it can only partially depict the complex way cells communicate with each other. It certainly does not represent the complexity of the human pulmonary epithelium and may misrepresent the toxic potential of nanomaterials, for better or for worse.
“Though animals will still be needed in research for the foreseeable future, ‘3D’ organoids nevertheless are an exciting prospect in our research field and in research more generally as a human equivalent and animal alternative.”

