It has long been known that people can form defenses and thus antibodies against viruses. But antibodies can also develop against polyethylene glycol (PEG), a substance used in cosmetics, food and medicine. These influence the effectiveness of drugs.
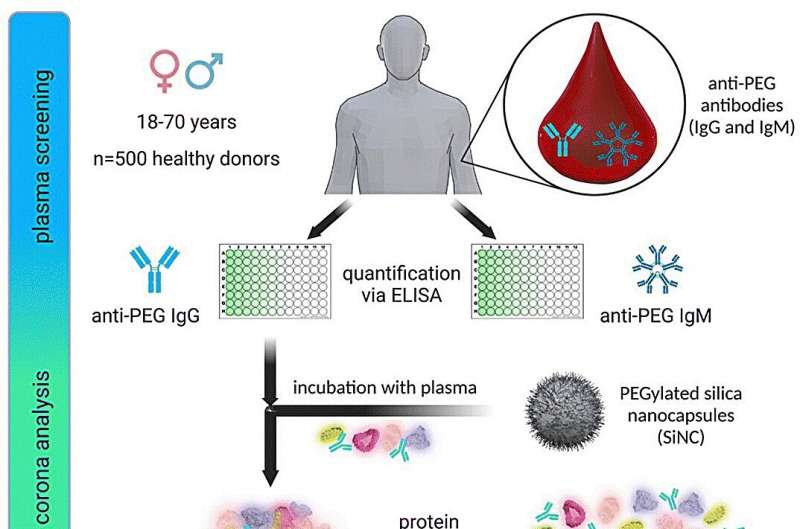
A team of researchers from the Max Planck Institute for Polymer Research has now investigated how widespread these antibodies already are in German society and how they might influence medical therapies using nanocarriers. They have published their current results in Nanoscale Horizons.
A virus invades the body and the immune system begins to work: Antibodies develop that fight the infection. At the same time, an immune memory builds up so that antibodies can be quickly made available in the event of a new infection. Surprisingly, antibodies can also form against polyethylene glycol (PEG), a molecule with a fairly simple structure.
In addition to cosmetic products—from creams, perfumes and lotions to lipstick—polyethylene glycol is also used in medicine. Here, it serves as a kind of camouflage coat against the body’s own immune system, thus increasing the circulation time of an active ingredient in the blood.
“For us, PEG is interesting for coating nano-sized drug carriers with it,” says Svenja Morsbach, group leader in Katharina Landfester’s department at the MPI for Polymer Research. In this way, the researchers achieve a longer circulation time for the drug capsules, which are only nanometers in size and could be an important component in novel cancer therapies in the future, for example.
In their studies, the team led by Morsbach and Landfester examined more than 500 blood samples from patients taken in 2019. “The antibodies formed against PEG attach themselves to the coated nanocarriers, thus counteracting the effect that is actually desired: the nanocarrier becomes visible to the immune system and is removed before it can exert its effect,” explains Katharina Landfester, director of the department.
The researchers led by Morsbach and Landfester assume that therapies will have to be adapted in the future to respond to this behavior of the immune system. In their statistical studies of blood samples, they found that PEG antibodies were already detectable in 83% of the samples examined.
The concentration of PEG antibodies in the blood correlates anti-proportionally with the age of the person examined: the older the person, the fewer PEG antibodies were present. “We currently assume that this is due to the increasing use of PEG in various areas of life only recently and the variation of the immune system in age,” says Morsbach.
In further studies, the researchers would now like to find out how future therapies could be adapted to compensate for the reduced camouflage of the nanocarriers. “Ideas would include whether PEG can be replaced or possibly dispensed with altogether,” Morsbach said. But determining the antibody concentration in a patient’s blood and individually adjusting the amount of active ingredient could also be an alternative.