Engineers at the University of California San Diego have developed an experimental vaccine that could prevent the spread of metastatic cancers to the lungs. The key ingredients of the vaccine are nanoparticles—fashioned from bacterial viruses—that have been engineered to target a protein known to play a central role in cancer growth and spread.
In mice, the vaccine significantly reduced the spread of metastatic breast and skin cancers to the lungs. It also improved the survival rate in mice with metastatic breast cancer after surgical removal of the primary tumor. The findings were published on Oct. 16 in Proceedings of the National Academy of Sciences.
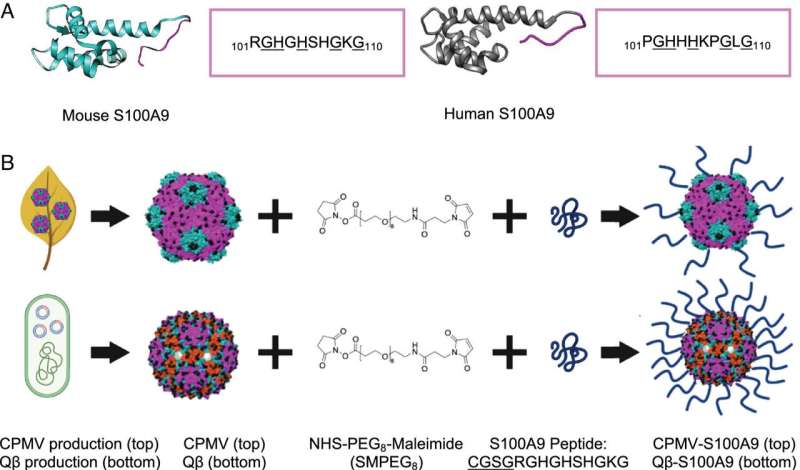
Metastasis is a process involving the migration of cancer cells from their primary site to other parts of the body. Recent studies have identified S100A9, a protein typically released by immune cells, as a key player in this process. Its normal role is to regulate inflammation. However, an excess of S100A9 can attract cancer cells like a magnet, causing them to form aggressive tumors and facilitating their spread to other organs, such as the lungs.
A team led by Nicole Steinmetz, a professor of nanoengineering at the UC San Diego Jacobs School of Engineering, developed a vaccine candidate that can modulate the levels of S100A9 when it goes haywire. When injected subcutaneously, the vaccine stimulated the immune system in mice to produce antibodies against S100A9, effectively reducing the protein levels and minimizing cancer metastasis to the lungs. The vaccine also increased the expression of immune-stimulating proteins with anti-tumor properties, while decreasing the levels of immune-suppressing proteins.
“S100A9 is known to form what is called a premetastatic niche within the lungs, creating an immunosuppressive environment that allows for tumor seeding and growth,” said study first author Young Hun (Eric) Chung, a UC San Diego bioengineering Ph.D. alumnus from Steinmetz’s lab. “By reducing S100A9 levels, we can effectively counteract the formation of this premetastatic niche, leading to a reduced attraction and increased clearance of cancer cells to the lungs.”
“This is a clever, new approach to vaccination in that we are not targeting tumor cells, but rather the tumor microenvironment so that it prevents the primary tumor from making new tumors,” said Steinmetz, who is the founding director of the UC San Diego Center for Nano-ImmunoEngineering and co-lead of the university’s Materials Research Science and Engineering Center (MRSEC). “We are essentially changing the whole immune system to be more anti-tumor.”
How it works
The vaccine consists of nanoparticles made from a bacterial virus called Q beta. The nanoparticles were grown from E. coli bacteria and isolated. Afterwards, a piece of the S100A9 protein was attached to the surface.
How it works is that the Q beta virus nanoparticles act as bait for the immune system. This virus is harmless to animals and humans, but immune cells recognize it as foreign and get fired up to attack to search for a pathogen. When the immune cells see that the virus nanoparticles display a piece of the S100A9 protein, they produce antibodies to go after that protein.
An advantage of using antibodies, Steinmetz noted, is that they help keep the levels of the target protein in check.
“With this form of immunotherapy, we are not necessarily knocking out all of the protein, but we are reducing the levels everywhere,” said Steinmetz.
Testing the vaccine candidate
The vaccine was tested in metastatic mouse models of melanoma and triple-negative breast cancer, an aggressive and hard-to-treat cancer type. Healthy mice were first administered the vaccine, then challenged with either melanoma or triple-negative breast cancer cells through intravenous injection. Vaccinated mice exhibited a significant reduction in lung tumor growth compared to unvaccinated mice. In unvaccinated mice, the injected cancer cells circulated throughout the body and eventually homed in on the lungs to form metastatic tumors.
The researchers note that this vaccine strategy combats tumor spread, not the primary tumor itself.
“While S100A9 does get overexpressed in certain primary tumors, it is mainly indicated in metastatic disease and progression,” said Chung. “The protein is involved in the formation of immunosuppressive tumor microenvironments. Therefore, we found that our vaccine is much more effective at reducing metastasis, and not in reducing the growth of the primary tumors.”
Another set of experiments demonstrated the vaccine’s potential to offer protection against cancer metastasis after surgical removal of the primary tumor. Mice with triple-negative breast cancer tumors who received the vaccine post-surgery demonstrated an 80% survival rate, while 30% of unvaccinated mice survived after surgery.
“These findings are the most clinically relevant, as they closely model what could happen in real-life scenarios,” said Steinmetz. “For instance, a patient diagnosed with an aggressive cancer who undergoes surgery to remove their tumor may be at risk of recurrence and metastasis to the lungs. We envision that this vaccine could be administered post-surgery to prevent such recurrence and outgrowth of metastatic disease.”
Next steps
Before the vaccine can progress to human trials, more comprehensive safety studies are needed.
“S100A9 is an endogenous protein within the lungs, and there aren’t a lot of data out there that demonstrate what happens when S100A9 is abolished,” said Chung. “We know that S100A9 is important in the clearance of pathogens, and future studies should better test whether reducing S100A9 levels decreases the patient’s ability to fight infections, especially in cancer patients who may have weakened immune systems.”
Future work will also explore the vaccine’s effectiveness when combined with other cancer therapies, with the aim of improving its efficacy against hard-to-treat cancers.