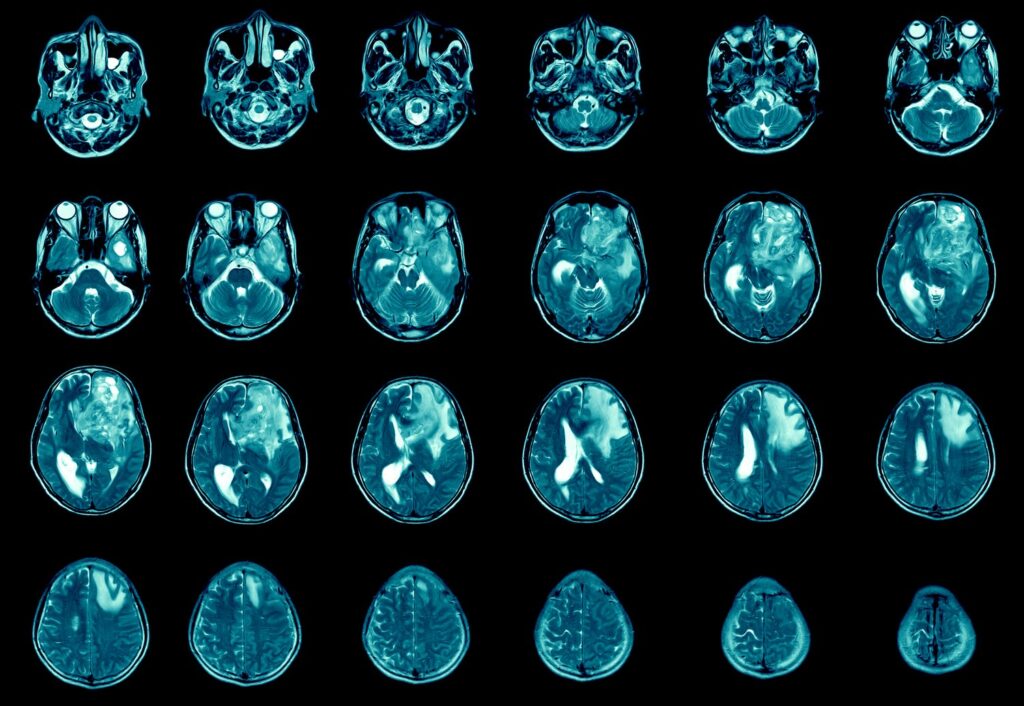
The battle against glioblastoma, a highly aggressive form of brain cancer, has been nothing but challenging. The prognosis for patients remains bleak, with average survival times scarcely exceeding one year.
Despite medical progress, mortality rates stay alarmingly steady. Despite this, a new approach is being studied. It might offer a different option for many patients facing this challenging disease.
Developed by a team of interdisciplinary scientists from the University of Toronto and Toronto’s Hospital for Sick Children, a new methodology aptly termed “mechanical nanosurgery” is shaking up the status quo. As revealed in the renowned journal Science Advances, preliminary results from a mouse model are encouraging.
Overcoming Resistance: The Potential of Mechanical Nanosurgery in Glioblastoma Treatment
The innovation involves the utilisation of carbon nanotubes (CNTs) loaded with magnetic iron nanoparticles and labelled with an antibody targeting a specific protein, CD44, abundantly found in many glioblastoma tumours.
Following injection into the brain region populated with drug-resistant glioblastoma cells, the CNTs start to rotate under the influence of a magnetic field. This disruption of cellular structures, both within and outside the cells, effectively kills off the cancerous cells, leading to enhanced survival rates in treated mice.
The possibility for application of this method is wide-ranging. Primarily, the technique could serve as a lifeline for those patients for whom traditional therapies, such as surgical intervention, radiation therapy, or chemotherapy with temozolomide, have failed due to developed resistance. In addition, the methodology could be customised to target different types of cancers.
Globally, the market for cancer therapeutics is anticipated to reach $335.06 billion by 2029, growing at a compound annual growth rate (CAGR) of 9.1%, according to a report by BioSpace.
Yet, the journey has its hurdles. The regulatory requirements for human trials, high research and development costs, the efficacy of the method on larger human brains and more complex tumours, and the potential risk to healthy brain cells are all significant challenges. There is no clear timeline for when this treatment might be ready for human trials.
Despite these obstacles, organisations like Cytimmune Sciences, specialising in versatile tumour-targeted therapies, have progressed. They’ve received over $11 million in investment, signalling a surge in funding for this promising field.
Conclusion:
While the leap from the lab to the clinic may not happen imminently, the introduction of mechanical nanosurgery into the armamentarium of cancer therapeutics signifies a potential watershed moment in the fight against glioblastoma. Despite the hurdles, with continued research and adequate funding, this innovation could lead the charge toward a new era of cancer treatment, offering renewed hope for patients across the globe.