Penn Engineers have modified lipid nanoparticles (LNPs)—the revolutionary technology behind the COVID-19 mRNA vaccines—to not only cross the blood-brain barrier (BBB) but also to target specific types of cells, including neurons. This breakthrough marks a significant step toward potential next-generation treatments for neurological diseases like Alzheimer’s and Parkinson’s.
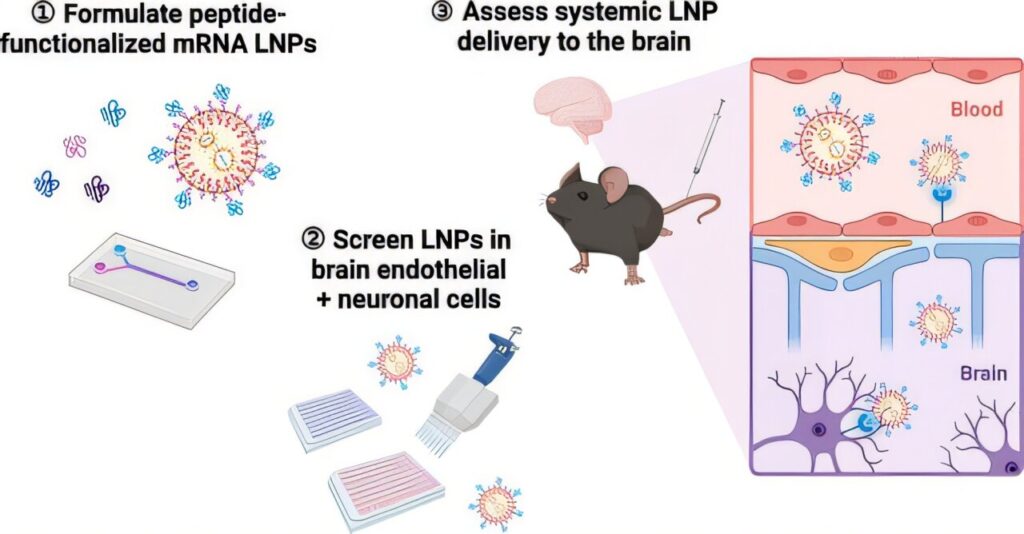
In a new paper in Nano Letters, the researchers demonstrate how peptides—short strings of amino acids—can serve as precise targeting molecules, enabling LNPs to deliver mRNA specifically to the endothelial cells that line the blood vessels of the brain, as well as neurons.
This represents an important advance in delivering mRNA to the cell types that would be key in treating neurodegenerative diseases; any such treatments will need to ensure that mRNA arrives at the correct location. Previous work by the same researchers proved that LNPs can cross the BBB and deliver mRNA to the brain, but did not attempt to control which cells the LNPs targeted.
“Our first paper was a proof-of-concept lipid nanoparticle design,” says Michael J. Mitchell, Associate Professor in Bioengineering (BE) and the paper’s senior author.
“It was like showing we could send a package from Pennsylvania to California, but we had no idea where in California it would end up. Now, with peptides, we can address the package to specific destinations with shared features, like every house with a red mailbox.”
The challenge of accessing the brain
Crossing the BBB is difficult because the structure has evolved to keep out virtually any dangerous or foreign molecules, including most medicines; mRNA molecules are too large to penetrate the barrier, as are most pharmaceuticals. The BBB also actively expels materials it deems hazardous.
“You can inject a treatment directly into the brain or spine, but these are highly invasive procedures,” says Emily Han, a doctoral student in the Mitchell Lab and the paper’s first author.
Because the BBB allows fat-soluble molecules through (like alcohol and THC, which is why those substances affect the brain), certain formulations of LNPs, which are partially made of the same family of fatty compounds found in everyday oils, can sneak through into the brain.
Peptides vs. antibodies
Until now, most research on targeting specific organs with LNPs has focused on combining them with antibodies, large proteins that function like biological nametags. “When you put antibodies onto LNPs, they could become unstable and larger in size, which makes it really hard to squeeze through the barrier,” says Han.
In contrast to antibodies, which can be hundreds of amino acids in length, peptides are just dozens of amino acids long. Their smaller size means they’re not only easier to place in large numbers onto LNPs but cheaper to manufacture. Peptides are also much less likely than antibodies to aggregate during LNP formulation or to provoke unintended immune responses.
The choice to use peptides started with an unexpected encounter between Han and a bat that flew into her room, potentially exposing her to rabies. While researching the vaccines she received against the disease, Han learned that one of the ways the rabies virus crosses the BBB is through the rabies virus glycoprotein.
“I then stumbled across one of our most promising targeting peptides,” Han says, a molecule known as RVG29, a 29-amino-acid segment of that protein.
Testing the concept
To confirm the peptides were functioning as intended, the researchers first needed to verify they adhered to the LNPs. “Our LNPs are a complex mixture of nucleic acids, lipids and peptides,” says Han. “We had to optimize quantification methods to pick out the peptides against all those other signals.”
Once they knew the peptides had adhered to the LNPs, the researchers then had to determine whether or not the peptide-functionalized LNPs (pLNPs) actually reached the intended targets in animal models.
“It’s really difficult to set up,” says Han, “because in the brain, you have so many different cell types and a lot of fat that can interfere with measurements.”
For more than six months, Han painstakingly developed a protocol to carefully take apart brain tissue, almost like a mechanic disassembling an engine.
Future directions
Next, the team aims to determine what fraction of neurons must be treated with pLNPs to meaningfully alleviate symptoms or potentially cure neurological diseases. “Returning to the same analogy, do we need to send these to every house with a red mailbox, or just 10% of them? Would 10% of neurons be enough?” asks Mitchell.
Answering this question will guide the development of even more efficient delivery strategies, bringing the promise of mRNA-based treatments for Alzheimer’s, Parkinson’s and other brain diseases closer to reality.