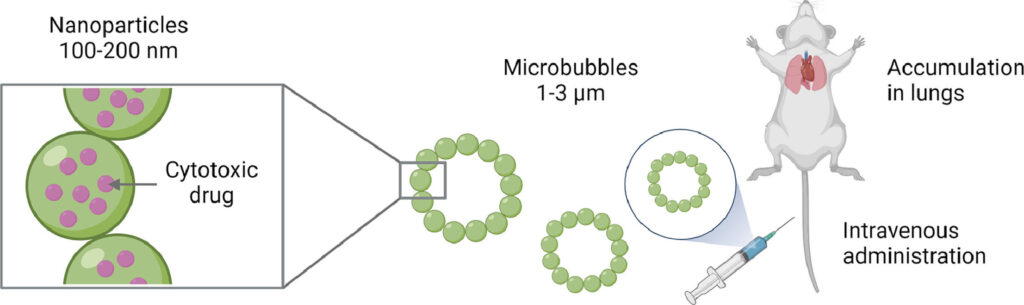
The delivery of nanomedicines using gas bubbles has shown itself to be a unique way of transporting cytotoxins to the lungs of cancer patients. The method enables precise and focused treatments, and the local action of the drugs also prevents a range of side-effects.
Results from SINTEF’s experiments with mice have shown that the impact of this form of medication is significant. Tumors were significantly reduced in size after only 30 days following the start of treatment.
The study has recently been published in the European Journal of Pharmaceutical Sciences, and the method is so promising that the research team has taken out a patent. SINTEF has also signed a license agreement with a pharmaceutical company.
“We’re very confident that this approach may offer us a new cure for lung cancer,” says researcher and Project Manager Andreas Åslund, who works at SINTEF’s Department of Biotechnology and Nanomedicine.
From a drawback to a benefit
It was in many ways something of a coincidence that this technology should end up as a lung cancer medication. Originally, the research team was working to identify a method that would deliver drugs to the brain. This is particularly difficult because the brain is enclosed in a separate membrane called the blood–brain barrier.
In other words, methods other than delivering drugs via the bloodstream are required in order to reach brain tumors. The researchers have addressed this problem by manufacturing gas bubbles that enclose the nanocapsules containing the drugs. The bubbles make it possible to use ultrasound to explode the nanocapsules, enabling the drugs to be “shot” through the blood–brain barrier.
So, at what scale are the researchers actually working? This is nanoscale—so small that as many as 100 nanocapsules, containing the drugs and enclosed in their gas bubbles, can sit across the width of a human hair. This being said, the drug itself constitutes only 10% of the package.
“After a while we discovered that these gas bubbles ended up in the patients’ lungs,” explains Åslund. “In the first instance, an accumulation of gas bubbles here wasn’t what we wanted, but the discovery meant that we could turn the problem upside down and instead exploit the phenomenon to reach tumors in the lungs,” he says.
Into the capillary network
The reason that this medication is so well suited to treatment of the lungs is that it takes place at nanoscale. All intravenous drugs enter the bloodstream and pass through the heart before they reach the lungs, where the vessels develop into what is called the capillary network.
Here, the vessels are very narrow and act as a filter for the microbubbles, which explode spontaneously and so deliver the nanoparticles containing the drugs directly into the lung tissue. Because the bubbles burst spontaneously, there is no need to use ultrasound to free the nanoparticles from their capsules in the capillary network.
The idea for this very specific form of medication emerged in the same department at SINTEF as early as in 2014. A decade of research work has led to many medicinal innovations. These include a drug delivery platform for the treatment of peritoneal cancer, which resulted in the spin-off company NaDeNo. And today, a new cure for lung cancer is on the researchers’ agenda.
Delivering drugs at nanoscale means that treatment is more gentle on the patient. “Nanomedicines have the benefit of acting very locally,” says Åslund. “This makes it possible to treat only the diseased tissue, and also enables us to administer stronger drugs.
“In so doing, we don’t have to worry about the drugs damaging healthy tissue. It also means that the patient will not suffer as many side-effects. It would in fact be very dangerous to administer drugs of this efficacy if the doses weren’t so minute,” he emphasizes.
This technology makes it possible to deliver more than just cancer drugs to the lungs. “We envisage that this method of drug delivery can also be used to treat other lung conditions such as cystic fibrosis, infections and pulmonary emphysema,” says Åslund.