Inflammation of the arteries is a primary precursor and driver of cardiovascular disease—the No. 1 killer of people in the United States. This inflammation is associated with the buildup of dangerous plaque inside the arteries. Advanced treatments are needed to target this inflammation in patients. Michigan State University researchers have tested a new nanoparticle nanotherapy infusion that precisely targets inflammation and activates the immune system to help clear out arterial plaque.
The research is published in the journal Nature Communications.
“There are two different things that people seem to be scared of when it comes to plaques,” said Bryan Smith, an associate professor with the Department of Biomedical Engineering in the College of Engineering and MSU’s Institute for Quantitative Health Science and Engineering. “Many people don’t really understand the difference between them.”
The first example is when your artery becomes blocked (for example, a 95% to 99% blockage). Often, there are symptoms like pain or pressure in the chest or nausea and dizziness beforehand and doctors will put a stent in the artery to increase blood flow. The second is when the plaque is highly inflammatory. This can make the plaque vulnerable to rupture, which can lead to artery blockages elsewhere in the body.
“That’s the scarier one that leads to most heart attacks,” said Smith. “Because such plaques don’t necessarily block much of the artery, and because the effects of the rupture can very suddenly completely block blood flow, such a heart attack can seem to appear as if from nowhere.”

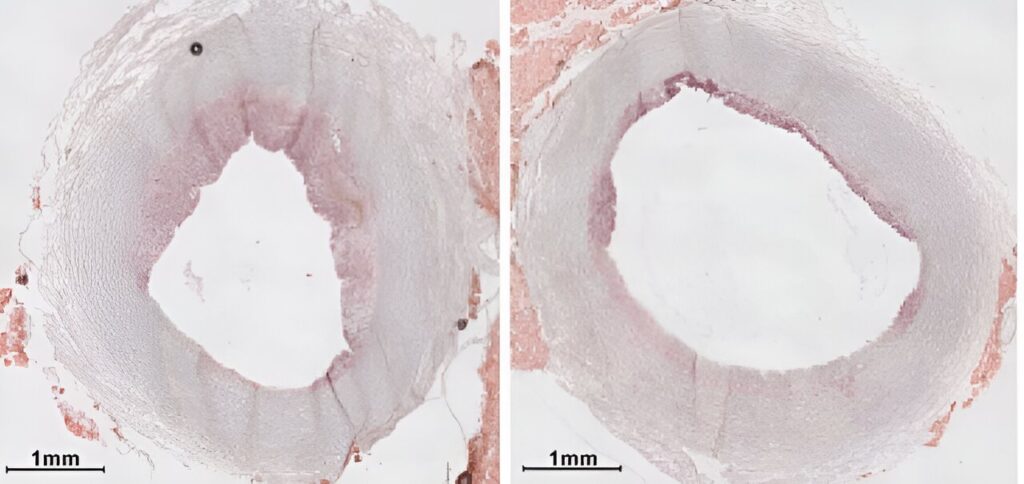
Smith and his team, including co-first authors postdoctoral fellows Yapei Zhang and Manisha Kumari, created nanoparticles—materials that are thinner than a human hair—that they used to develop a nanotherapy infusion. The nanotherapy selectively targets a specific immune cell type that moves into and is a part of the plaque. These treated cells “eat” away parts of the plaque core, removing it from the artery wall and decreasing levels of blood vessel inflammation.
Previous studies by Smith and his collaborators, the Leeper Lab at Stanford University, tested the infusion on mice and now, pig models, to prove the infusion’s effectiveness, and critically, its lack of side effects due to its precision immune targeting.
“Using PET [positron-emission tomography] scans, we were able to measure the effects of the therapy on pig arteries,” said Smith. “We showed in animal models such as pigs that we can decrease the levels of inflammation in the plaque based not only on this clinically used PET imaging technique but also by molecular assays. Just as importantly, we saw none of the side effects that would have been anticipated had the therapy not been precisely targeted.”
Earlier studies in mice required hundreds of microliters of the nanotherapy infusion, but most recently, Smith and his team have achieved a measurable impact in pigs by scaling up the amount produced to liters. These volumes are in the range needed for human use. This study represents a critical step toward translation to patient clinical trials of safer, more effective cardiovascular therapies.